
 The Bertoletti lab would work flat out through the Circuit Breaker, digging beyond antibodies to discover more about the immune system’s response to SARS-CoV-2.
The Bertoletti lab would work flat out through the Circuit Breaker, digging beyond antibodies to discover more about the immune system’s response to SARS-CoV-2.
“We deal with hepatitis B, so we don’t usually see such a big response,” explains Ms Kamini Kunasegaran, a research assistant with Professor Antonio Bertoletti’s laboratory at Duke-NUS, about her team’s
first foray into studying SARS-CoV-2. “The SARS-CoV-2 response was really big.”
“That really was the turning point,” adds her lab mate Ms Adeline Chia, a senior research associate. “Everyone got so excited.”
Kamini and Chia were referring to the first quantitative glimpse their team, which is part of Duke-NUS’ Programme of Emerging Infectious Diseases, gained into the body’s
T-cell response to the virus on the eve of Singapore’s Circuit Breaker.
Unlike the response to chronic hepatitis B virus (HBV), studying SARS-CoV-2 yielded entirely different results.
“The ELISpot lit up like a Christmas tree,” says Kamini referring to the test they had performed to count SARS-CoV-2-specific T cells.
The test revealed a clear and robust T-cell immune response. After shaking off doubts that something had gone wrong, the team felt excited. And Twitter’s agreement was immediate and emphatic: this was indeed exciting.
The discovery would launch a three-month sprint to a Nature paper.
Working in the new (ab)normal
Of course, such breakthroughs — and their accompanying tweets — are highlights which reveal little of the arduous research process that generated them.
Before the pandemic, the team had been investigating the behaviour of T cells in a body with chronic HBV infection. T cells are immune cells that recognise and target foreign invaders once these have squirrelled their way into the body’s cells.
In chronic HBV infections, the continued presence of the virus elicits a countermeasure response from the body’s T cells, which continue to patrol the bloodstream in low numbers; perhaps one per 10,000 T cells was on the lookout for HBV. With
neither side winning, the body reaches a stalemate that the team had been investigating.
But when SARS-CoV-2 struck, the team quickly turned their well-honed expertise to studying T cells in SARS-CoV-2 infections. While that pivot posed no technical difficulties to them, the team had to adapt to the challenges of an unprecedented
pandemic.
With the Circuit Breaker looming ahead of them, having everyone together in the laboratory was off the table; this at the precise moment when they needed all hands on deck. Instead, the lockdown and its associated safe distancing measures would
whittle the on-site team down to a crew of eight.
“It was chaos in the beginning,” recalls Kamini, who was assigned to the skeleton crew that would work in the lab over the months to come.
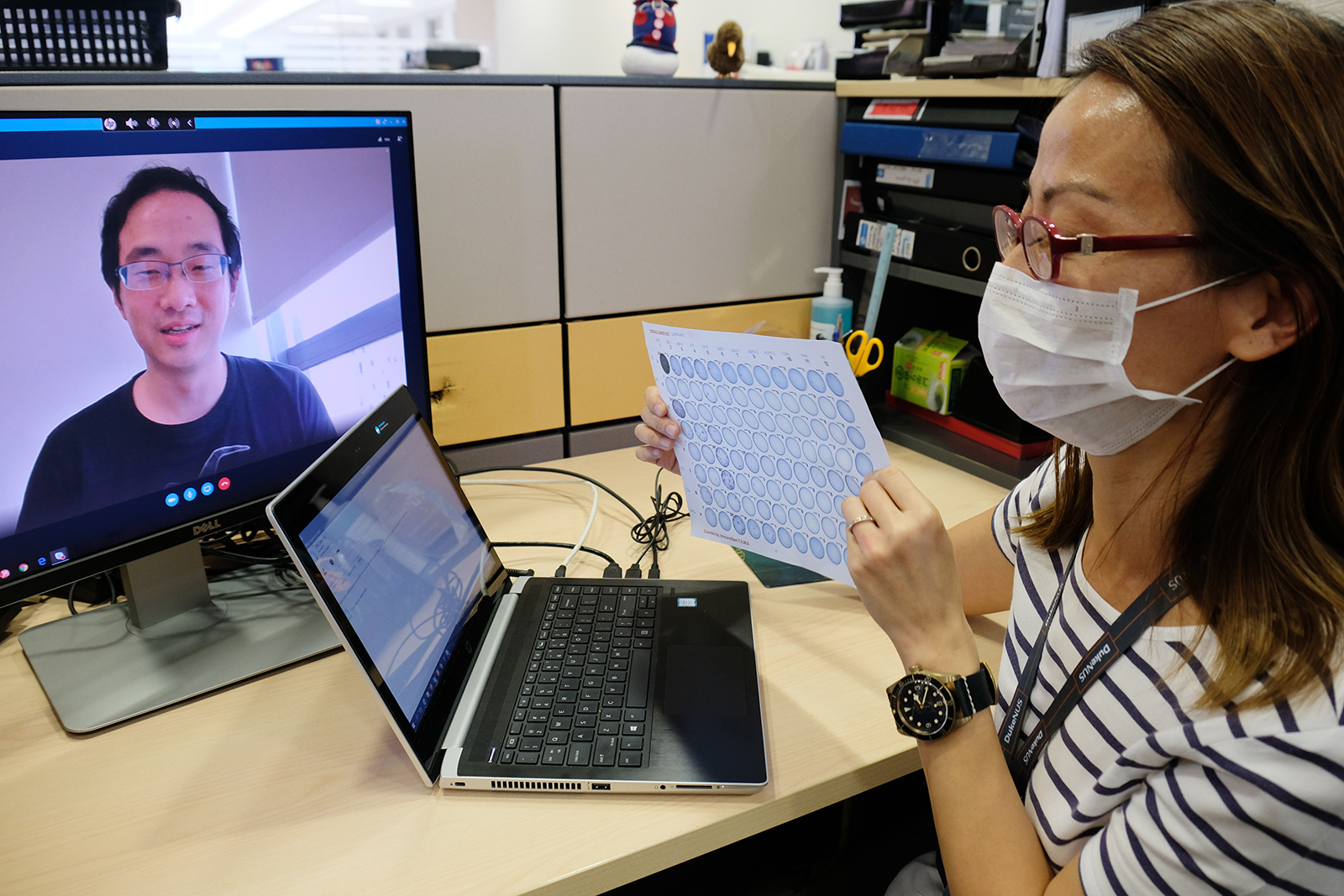
DURING THE CIRCUIT BREAKER, THE TEAM EXERCISED THEIR CREATIVITY TO ENSURE FAST AND EFFECTIVE COMMUNICATION BETWEEN THOSE IN THE LAB AND THOSE WORKING REMOTELY
Those who would be allowed back into the lab were further divided into morning and afternoon shifts. Getting their work done in that short span of time would subject them to immense time pressure, and demand clear communication. The team would
have to keep in close contact, so they could easily pick up from where the other shift had left off.
“Having a long enough working relationship was important for times like these,” stresses Chia, who coordinated the on-site team.
It would turn out to be a steep learning curve. Even while they navigated the impending new restrictions, the pace of research accelerated. Studying SARS-CoV-2, unlike HBV, meant responding to a dynamic and unpredictable situation.
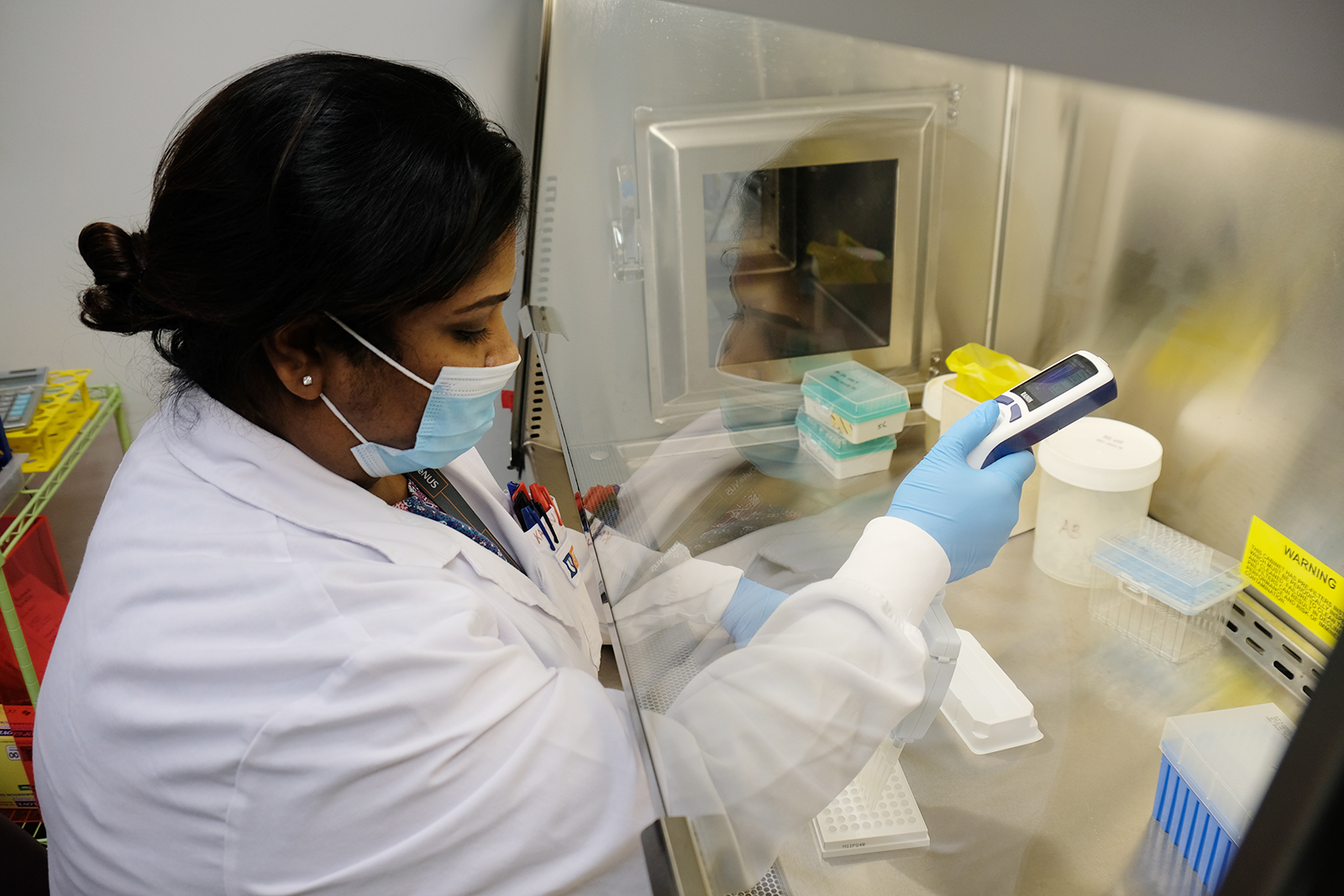
KAMINI WORKED THROUGHOUT THE CIRCUIT BREAKER, ISOLATING AND STUDYING T CELLS IN PATIENT SAMPLE
And unlike the frozen HBV samples the team was used to handling, they were working with fresh blood samples. That meant time was of the essence.
“We had to collect the samples, process them and then do the experiments straight away,” explains Kamini. “If the sample came in at 5pm, in our HBV work, we could have left it till the next morning before starting our
experiments. But with fresh samples, we had to process them immediately.”
Processing alone would take about two hours and only then could they start with their experiments which would take another three hours. Long shifts would become the norm.
With the samples coming directly from patients at Singapore General Hospital and other collaborating institutions across Singapore, the team also would not be able to anticipate the quantity and quality of samples on any given day. There
could be a glut, or not a single one. And without a scheduled pool of samples, they could not plan ahead. From day to day, the priorities for what to test in each set of samples would shift.
“It would all depend on the samples, and at that point, what question we wanted to ask,” says Kamini.
Chia chimes in: “Sometimes the decision could only be made on the spot, about what exactly we would do with these precious samples.”
An eye on immunity
That first discovery would open the floodgates to new opportunities.
“The project exploded,” says Chia. “We’re collaborating with even more people, and we have even more samples coming in. But the good thing is, our staff are even more well-trained.”
Novel mRNA vaccines would be introduced in a matter of months, opening another opportunity for the team to study the T-cell response. This time in healthy vaccinated individuals.
The team’s schedule, too, would eventually ease back to some semblance of normalcy. Indeed, the crucible of stress would forge a greater sense of cooperation among the team.
“The teamwork is more pronounced now,” reflects Chia. “We’re all working towards a common goal, and there is a lot of help between people.”
Chasing the blips of excitement
The tweet sent on the eve of the Circuit Breaker would culminate in a Nature paper titled “SARS-CoV-2-specific T-cell immunity in cases of COVID-19 and SARS, and uninfected controls”,
on which Kamini and Chia are both co-authors.
It’s one of those rare breakthrough moments — “the little blips of excitement” as Chia puts it.
Reflecting on the speed with which the study progressed — it went from idea to publication in just three months — Kamini remembers her surprise: “Whoa, that was fast.”
For Chia, this blip was all the more thrilling because it proved their strong collaborative spirit.
“It was the first time there were so many people from the lab in the paper. Looking back, it really does feel like a big collective effort.”