
 A veteran of high-containment labs returns to the hot zone just in time to sequence SARS-CoV-2.
A veteran of high-containment labs returns to the hot zone just in time to sequence SARS-CoV-2.
Ok, we can’t really mess this one up. That was molecular virologist Martin Linster’s main thought during those early weeks when he or one of his colleagues collected Singapore’s very first SARS-CoV-2 samples from across
the island.
The way he tells it, those errands were straight out of a heist movie.
“We got with a courier the first weeks of the outbreak. We went into the dispatch driver’s lorry just to make sure the samples were safe,” recalls Linster, a then-senior research fellow with the Emerging Infectious Diseases Programme at Duke-NUS.
During those times, the team’s circuit started at Singapore General Hospital around 3pm before proceeding to the basement loading bay of the National Centre for Infectious Diseases. At both stops, they’d swap iceboxes full of triple-sealed
patient samples for a signature.
Then, once they were suited up and fitted with a respirator, the team — including Linster — could examine the contents of their iceboxes in the safety of the biosafety level 3 (BSL3) lab.
Securing the cold chain
Linster had not planned to do BSL3 lab work when he moved to Singapore in the mid-2010s as a research fellow. He already had a decade’s worth of investigations within these high-security containment facilities under his belt; it’d be good,
he thought, to work elsewhere in the field of emerging infectious diseases after all that.
But after a few years, he started missing BSL3 work and it took little convincing for Linster to join his first Duke-NUS BSL3 project in 2019 — he was accordingly in prime position to contribute his expertise when the virus spread.
“You start up slowly again,” says Linster of his return. He had to re-acclimatise to the sealed-off environment of the BSL3 with its ventilation and noises — “it’s a bit like doing your first scuba dive,” he says. “Then
you go full speed when the pandemic hits.”
As a virologist, Linster’s work is vital for tackling how infectious diseases spread. He maps out the genetic sequences of viruses and studies how they infect cells, mutate and importantly for these uncertain days, multiply. His findings underpin
the work of other researchers who use these insights to develop treatments, therapies and vaccines.
Previously, Linster worked on “less newsworthy viruses” when he studied human parainfluenza virus in Vietnamese children in 2009. Linster’s analysis showed that a particular strain was responsible for most of the cases, and that diverse
virus strains were entering Vietnam.
In 2014, Linster researched how far away an H5 avian influenza is from mutating into an airborne pathogen that readily spreads among its hosts. He found that five positions in the viral genome could be changed so that the virus binds to and infects cells
of the new host.
With all this research expertise, Linster was a natural choice to join the team assigned to culture the virus within the BSL3. These cultures would give other scientists a ready supply of the virus for their work.
Here, the courier journeys, iceboxes, and strictly regulated BSL3 were necessities — the Duke-NUS team’s work called for samples and security.
“The question was really, how good was your patient sample?” Linster explains. “Did you manage to keep the cold chain?”
Maintaining the cold chain in this case meant keeping the virus and cells in the samples from SARS-CoV-2 patients alive at a low temperature.
Break the chain, though, and the virus dies. SARS-CoV-2, it turned out, is pretty unstable outside the human body in tropical Singapore.
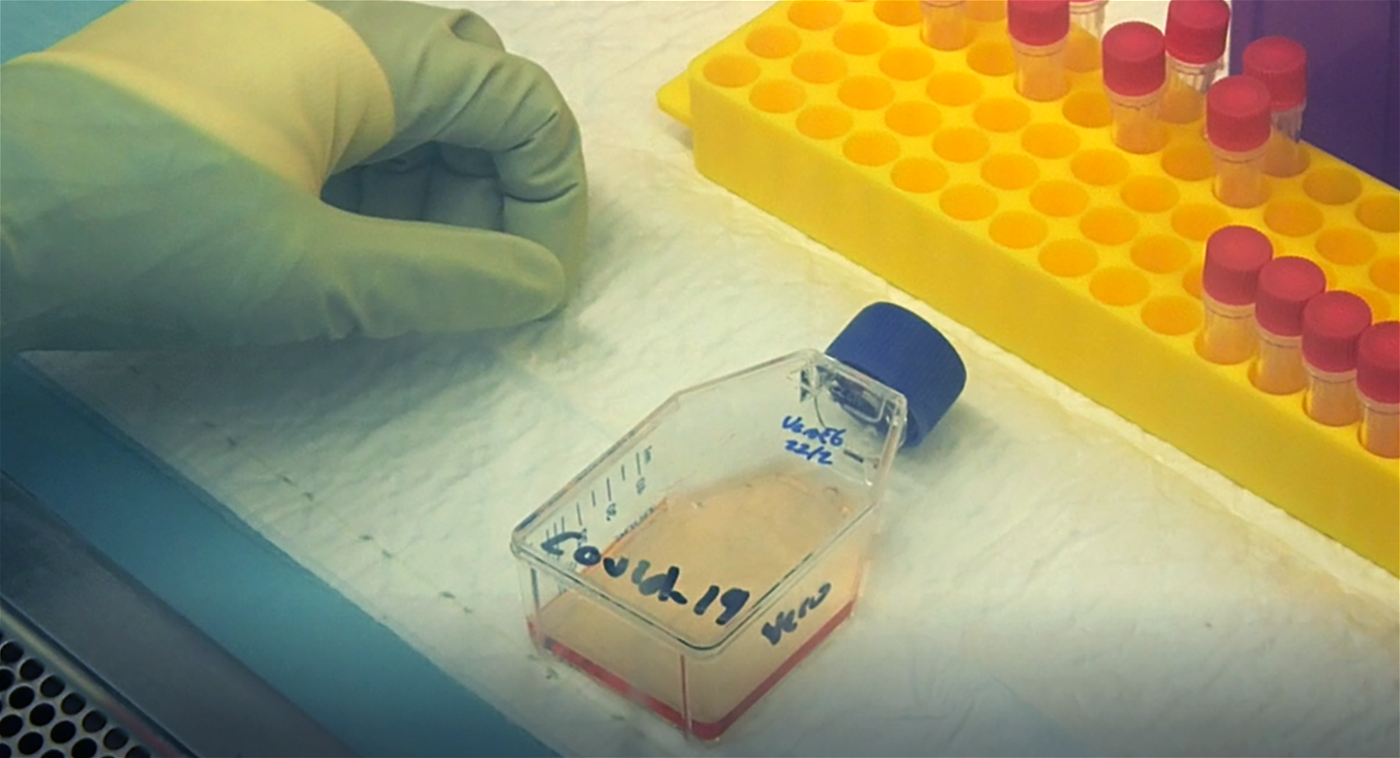 A MEMBEr OF THE DUKE-NUS TEAM WORKS IN THE BSL3 LAB ON ISOLATING THE NOVEL CORONAVIRUS
A MEMBEr OF THE DUKE-NUS TEAM WORKS IN THE BSL3 LAB ON ISOLATING THE NOVEL CORONAVIRUS
After some initial fine-tuning of the experiments, a clear pattern emerged. The team put the virus samples into a carefully selected cell line that allowed the virus to infect the cells and replicate in order to document the effect of infection.
“You look under the microscope,” says Linster. “And you see cell death.”
Cracking the code
This pattern was not necessarily unwelcome. It was what virologists term a “cytopathic effect”. This is when a pathogen invades and causes structural changes in an affected cell.
And Linster and the team didn’t just see their cells die. They watched them bursting all over each other. Such an uncontrollable and messy death typically results from a major injury to cells and is consistent with how viruses affect them.
This was a key clue. Now, they had to wait for their tests to finish running to make sure that this was indeed the work of a virus.
“You think ‘OK, this doesn’t look normal, but was there a bacterial contamination or anything?’” he remembers.
“Then you look at the screen for half an hour to just convince yourself and the rest of the world that this is really positive if you do it over again. Because you could’ve done something wrong.”
In the end, the team’s findings proved accurate; yes, this was all indeed the work of a virus, and here was its genetic code in full. It had taken the team less than a week to complete this feat, which would unlock opportunities
for the rest of the scientists at Duke-NUS and beyond to develop tests, treatments and vaccines.
With such an important discovery in their possession, the team was swift to publish their data. They were only the third lab in the world to do so, after ones in China and Australia.
“As a scientist, you want to do something new, right?” he asks. “You say ‘Okay, I’m number three’? Personally, I’m not too much interested in being that hamster in the treadmill.”
A swifter response
Research papers and national and international collaborations resulted regardless.
“There were surprises every day. That was the essence of what kept us going,” says Linster.
For him, one of the most exciting projects to follow would be a collaboration with the lab of Antonio Bertoletti, a colleague and professor with Duke-NUS Emerging Infectious Diseases Programme, who specialises in the study of T cells.
“Characterising the T-cell response, we found something rather unexpected that would be met with strong interest from the world,” says Linster of what they would discover.
Exciting new opportunities aside, Linster believes that the lessons from this pandemic will help us respond more efficiently when future pandemics strike.
He also advocates that the global scientific community, and virologists in particular, should work together on an easily-accessible catalogue of crucial viral mutations that could underpin the next outbreak. It would be a timely tool for researchers
by researchers. Such a collaborative effort would, he expects, save lives during any future pandemic.
“It is a lot of effort, but it’s crucial,” muses Linster. “We seriously want to prevent the next pandemic from happening on a scale like the current one.”