Back
Monday, 26 Sep, 2022
Enhanced Primary Care Symposium, 22 August 2022
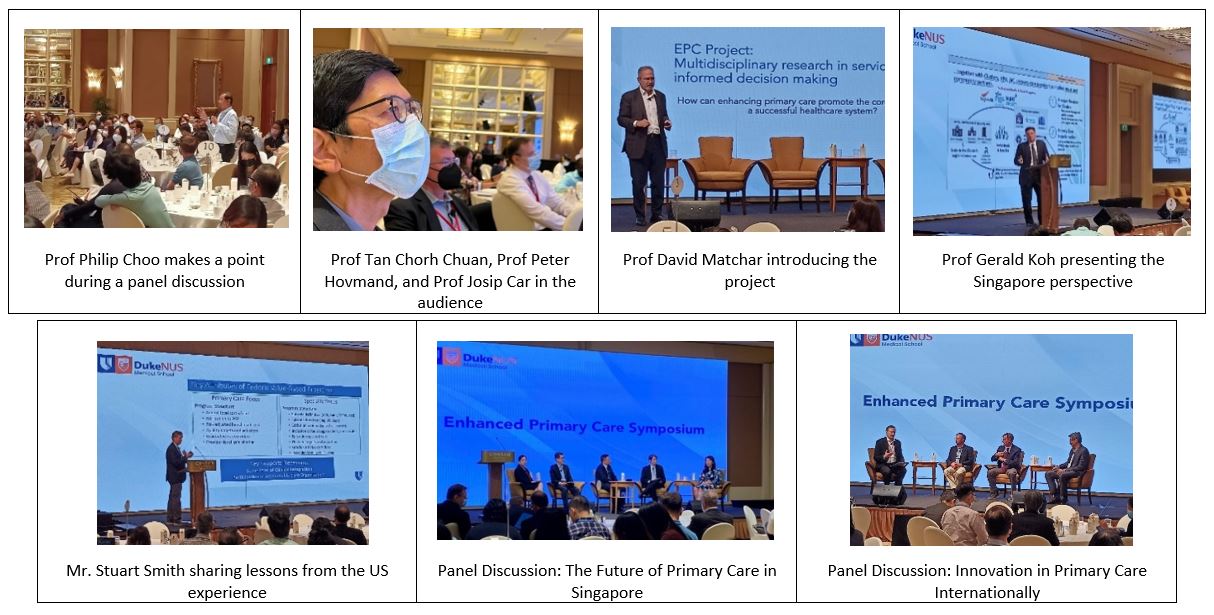
The Enhanced Primary Care (EPC) Symposium brought together primary care stakeholders including executives, administrators, practitioners, and researchers to discuss the context, findings and implications of the EPC research project, a three-year collaborative effort that features contributions from all three medical schools in Singapore.
Professor Tan Chorh Chuan, Chief Health Scientist of the Ministry of Health (MOH) and Executive Director of MOH Office for Healthcare Transformation (MOHT), gave the opening remarks. Professor Tan emphasized the need to distill the pivotal directions which can lead to successful primary care transformation. He pointed out that true enablement of primary care partners (PCPs) goes beyond advancing academic knowledge and clinical skills. A multi-layered ecosystem must be built that not only supports professional development, but allows PCPs to effectively manage clinical and social care needs and achieves functional integration with the rest of the healthcare system. Additionally, it is critical to engage communities, residents, patients, and their families to be on board with this movement. Finally, enablers such as accessible and connected IT and data systems, and revised financing structures are vital changes needed to allow PCPs to move away from high-volume episodic care and towards stable long-term care for patients with a strengthened focus on preventive health. He invited partners and thought leaders to come together to develop solutions for the success of HealthierSG.
Professor David Matchar, PI of EPC Project, explained how various components of Health Services Research (HSR) aim to translate policies into actions on the ground. Professor Matchar highlighted that Singapore’s health systems are under stress. We must understand where current problems and gaps lie and identify the necessary future steps to improve the delivery of primary care services. Policies must ultimately flow down to end provider practices, with the common goal of enhancing the “4Cs” (first contact access, comprehensiveness, continuity, and coordination) of primary care, hence reducing the extent to which needs remain unmet, and achieving higher levels on some dimensions of the “Quadruple Aim” (population health, unit cost, patient satisfaction and provider satisfaction).
Next, Co-PI Professor Prof Gerald Koh Choon Huat, Head and Clinical Director (Future Primary Care) of MOHT shared his views on the past, current and desired future trends of primary care in Singapore. Professor Koh described a life-course approach to drive population health in the HealthierSG reform. He emphasized that key system enablers and care protocols need to be designed with practical translation and implementation goals in mind. There must be awareness to better align incentives and interests of PCPs to work towards achieving HealthierSG goals.
Professor Koh then moderated a panel discussion on Future of Primary Care in Singapore with Dr David Ng (CEO, SingHealth Polyclinics), Dr Chong Phui-Nah (CEO, NHG Polyclinics), Dr Tham Tat Yean (CEO, Frontier Healthcare), and Dr Ruth Lim (Director, Primary & Community Care Division, MOH). Panelists shared that initiatives to strengthen primary care have been an ongoing effort, and it is encouraging that many of these will be incorporated in HealthierSG. Primary care cannot work in silos but requires full support and integration into current healthcare clusters and other established community partners. Policy and clinical care protocols must be endorsed by both PCPs and hospital specialists, but more importantly, they must also engage and factor in patient and resident requirements and needs.
Mr. Stuart Smith, Vice President of Finance at Duke University Health System, then spoke on his experiences working in developing an Accountable Care Organization (ACO) to bridge a fully integrated ecosystem consisting of both primary care providers and specialty providers. Patients present to various care sites in different stages of health; care management teams embedded at different sites have to develop their capacities to right-site patients for the best Quadruple Aim outcomes. Funding structures, data sharing, e-communication and analytics are essential to primary care enhancement and integration.
A second panel discussion on International Perspectives on Innovation in Primary Care was moderated by EPC project Co-PI Professor Josip Car of the Lee Kong Chian School of Medicine. The experts on the panel were Professor Peter Hovmand of Case Western Reserve University, Mr. Stuart Smith, and Dr. Piya Hanvoravongchai of Chulalongkorn University. The experts opined that while healthcare financing is essential, capitation models can undergo constant revision. Understanding of what patients and PCPs view to be an ideal sate of primary care in the local context is fundamental to driving primary care transformation. We must understand their values on healthcare outcomes and their perspectives on meaningful healthcare. This ultimately leads to the most important aspect of building lasting trust between patients and PCPs.
In the afternoon sessions, Professor Matchar first introduced the building blocks and linkages of the EPC project methodology. Then, project researchers presented four methods workshops in a non-technical and accessible style to explain the methods used, the findings and implications of their work. These sessions covered participative and community based model building (by Professor Peter Hovmand), epidemiological analysis of health states (by Dr Abhijit Visaria and Ms. Nirmali Sivapragasam), discrete choice experiments to assess provider and patient preferences (by A/Prof Semra Ozdemir), and system dynamics modeling of the impact of primary care interventions on of Singapore’s population, population health, health service utilization and healthcare costs (by A/Prof John Ansah).
In his closing remarks, Professor Matchar drew the attention of the audience to a common theme running across all the sessions: the need for integration, alignment, and communication between the primary care sector and the other sectors of the health system. He summarized the key take-aways from each of the sessions, and explained the rationale for investing in modelling as a support for policy making – when done well, modelling allows us to work together to achieve the core objectives of the health system.