Clinical features:
- Characterized by urge to move legs that may be accompanied by uncomfortable or unpleasant sensations in the legs
- Worsens during period of rest or inactivity
- Partially or totally relieved with movements
- Worse in the evening or night
It is a diagnosis of exclusion after excluding other medical or behavioral condition (e.g. myalgia, venous stasis, leg oedema, leg cramp, positional discomfort, habitual foot tapping).
Definitions:
Intermittent: bothersome symptoms that require treatment, on average occur less than twice per week
Chronic persistent: frequent and bothersome symptoms that require daily treatment, on average occur at least twice per week
Augmentation: drug-induced worsening of RLS (earlier onset, spread of symptoms to the arms, worsening of symptoms with dose increase, shorter effect of medication)
Refractory: Unresponsive to monotherapy of first-line agents due to adverse effects, augmentation or efficacy reduction
Causes:
- Iron deficiency
- Uraemia
- Hypoparathyroidism, hyperphosphataemia
- Sleep deprivation
- Medications
- antipsychotics (e.g. quetiapine)
- antidepressants (selective serotonin reuptake inhibitors [SSRIs], tricyclic antidepressants [TCAs], mirtazapine)
- carbamazepine
- lithium
- beta blockers
- first-generation antihistamines
- dopamine-receptor antagonists (e.g. metoclopramide)
- calcium channel blockers
Non-pharmacological management:
- Take warm or cool showers. Apply warm towel/ heating pad or cold compresses.
- Stretch and/or massage legs. May consider pneumatic compressions
- RLS during the day: listen to quiet, calming music or do activities that help relax or take mind away from the feelings of restlessness (e.g. doing puzzles)
- RLS at night: practice sleep hygiene
- Avoid or limit intake of caffeine, alcohol and nicotine
- Engage in physical activities during the day to help with sleep at night
- Engage in mental activities such as video games and crossword puzzles
- Practice good sleep hygiene
Pharmacological Management:
- Treat underlying cause if possible/ appropriate
| Available Drugs |
Dosing Regiment |
Side Effects |
Credanil 125mg (levodopa 100mg/carbidopa 25mg)
Sinemet CR 250mg (levodopa 200mg/carbidopa 50mg) tablet
|
Levodopa 100mg-200mg/day (increased risk of augmentation at ≥200mg/day)
|
Orthostatic hypotension (increased risk of falls), dizziness, weakness, insomnia, peripheral edema, cardiac arrhythmia, psychosis, augmentation
|
Codeine 30mg tablet
|
30-90mg before bed
|
Constipation, nausea
|
Tramadol 50mg tablet
|
50-100mg before bed
|
Constipation, nausea, occasionally associated with augmentation
|
Zopiclone 7.5mg tablet
|
Max: 3.75mg ON
|
Look out for excessive sedation
|
Zolpidem CR 6.25mg, 12.5mg tablet
|
6.25mg-12.5mg ON PRN
Max: 12.5mg ON
|
Benzodiazepine (e.g. lorazepam 1mg tablet)
|
PO 0.5mg-1mg ON PRN.
Max doses as below:
<65 years old: 2mg ON
≥65 years old: 1mg ON
|
Gabapentin 100mg, 300mg capsule
|
100mg ON (up to 300mg/day)
|
Drowsiness, dizziness
|
Pregabalin 25mg, 75mg capsule
|
25-75mg ON
Max dose: 75mg/day (as a single or 2 divided doses)
|
Ropinirole 0.25mg, 1mg, 2mg tablet
|
Start at 0.25mg ON (1-3hr before bedtime), may be increased after 2 days to 0.5mg daily, and after 7 days to 1 mg daily. Dose may be further titrated upward in 0.5 mg increments every week until a daily dose of 3mg during week 6 as tolerated and needed.
Max dose: 3mg/day
Taper dose if withdrawing treatment
|
Nausea, fatigue, giddiness
More likely to have orthostatic hypotension but less risk for augmentation compared to levodopa
Sleep attacks may be a class effect especially at higher doses; driving not recommended. Reduce dose immediately if sleep attacks occur.
Risk for impulse control disorder (average onset: 9 months)
For patients who require twice daily regimen (e.g. in mild augmentation), first dose may be taken in the late afternoon or early evening.
Do not discontinue abruptly.
|
Pramipexole 0.125mg tablet
|
0.125mg 2-3hours before bedtime. Double dose every 14 days up to 0.5mg. Attempt up to 0.75mg cautiously as population of CrCl<20 was not studied. Dose earlier, divide into multiple evening doses or increase dose if augmentation occurs.
(Gradual reduction every 4-7 days on discontinuation)
*risk of possible accumulation
|
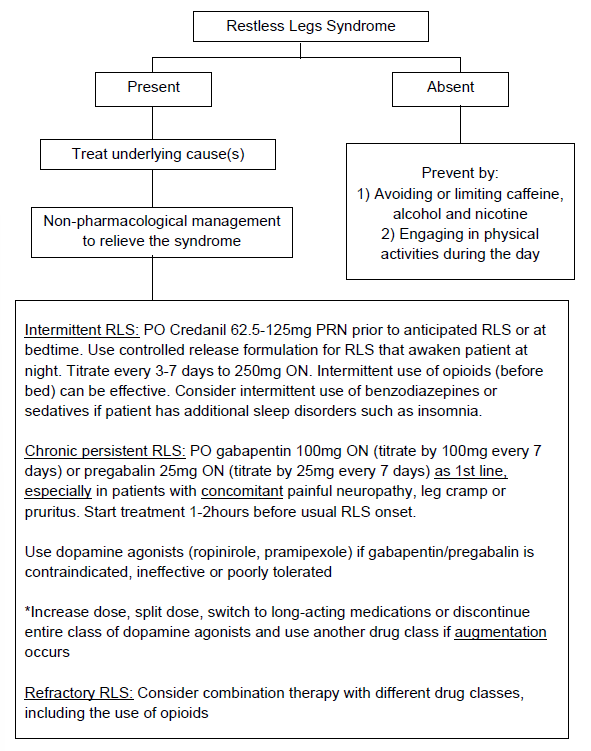
Treatment Algorithm
References
-
Silber, M. H., Buchfuhrer, M. J., Earley,C. J., Koo, B. B., Manconi, M., Winkelman, J. W., & Scientific and Medical Advisory Board of the Restless Legs Syndrome Foundation. (2021). The Management of Restless Legs Syndrome: An Updated Algorithm. Mayo Clinic proceedings, 96(7), 1921-1937. doi: 10.1016/j.mayocp.2020.12.026
- Giannaki, C. D., Hadjigeorgiou, G. M., Karatzaferi, C., Pantzaris, M. C., Stefanidis, I., & Sakkas, G. K. (2014). Epidemiology, impact, and treatment options of restless legs syndrome in end-stage renal disease patients: an evidence-based review. Kidney International, 85(6), 1275-1282. doi:10.1038/ki.2013.394
- Sahli, Z. T., Jo, J., Mousa, S. A., & Tarazi, F. I. (2017). Clinical management of restless legs syndrome in end-stage renal disease patients. CNS Spectrums, 22(01), 14-21. doi:10.1017/s109285291600064x
- Novak, M., Winkelman, J. W., & Unruh, M. (2015). Restless Legs Syndrome in Patients With Chronic Kidney Disease. Seminars in Nephrology, 35(4), 347-358. doi:10.1016/j.semnephrol.2015.06.006
- Scherer, J. S., Combs, S. A., & Brennan, F. (2017). Sleep Disorders, Restless Legs Syndrome, and Uremic Pruritus: Diagnosis and Treatment of Common Symptoms in Dialysis Patients. American Journal of Kidney Diseases, 69(1), 117-128. doi:10.1053/j.ajkd.2016.07.031
- Chambers, E. J., Germain, M. J., & Brown, E. A. (2010). Supportive care for the renal patient. doi:10.1093/acprof:oso/9780199560035.001.0001
- Symptom Assessment and Management. (2017, August). Retrieved February 01, 2018, from http://www.bcrenalagency.ca/health-professionals/clinical-resources/symptom-assessment-and-management
- Davison, S. N., Levin, A., Moss, A. H., Jha, V., Brown, E. A., Brennan, F et al. (2015). Executive summary of the KDIGO Controversies Conference on Supportive Care in Chronic Kidney Disease: developing a roadmap to improving quality care. Kidney International, 88(3), 447-459. doi:10.1038/ki.2015.110
- Lexicomp. (2018). Lexi-CLINICAL SUITE [Online database]. Retrieved from http://online.lexi.com/lco/action/home/switch?siteid=129