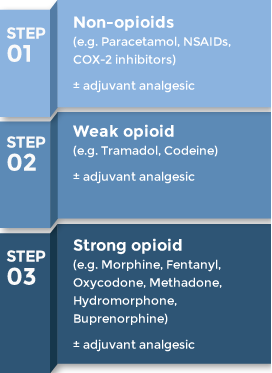
WHO’s pain ladder can be used as a guide for both cancer pain and pain in life-limiting progressive non-cancer conditions (e.g. end stage organ failures or progressive neurological conditions).
*Some patients (e.g. those with severe incident pain) may benefit from interventional analgesia - contact the relevant Chronic Pain service (by anaesthetists) in your institution.
Step 1: For mild pain
- Paracetamol 0.5-1g q.d.s.
- NSAIDs: Ibuprofen 400mg t.d.s., Naproxen sodium 275-550mg b.d., Diclofenac 50mg b.d./t.d.s.
- COX-2 inhibitors: Celecoxib 200mg b.d., Etoricoxib 60-120mg each morning
Step 2: For moderate pain, or if pain relief not achieved at maximum dose in Step 1
- Start weak opioid: either Codeine 30-60mg t.d.s./q.d.s. or Tramadol 50-100mg t.d.s./q.d.s
- Continue Paracetamol if it has been helpful, stop if pill burden is too much for patient.
Step 3: For severe pain, or if pain relief is not achieved at maximum dose in Step 2
- Start a strong opioid (e.g. Morphine, Fentanyl, Oxycodone).
Using Morphine
- Morphine remains the gold standard for strong opioids
- Oral Morphine is available in two forms:
- Normal release Morphine sulphate solution, also known as mist Morphine
- Starts working within 30-40 min and lasts 4 hours (if renal function is normal), usually available as 1mg/ml.
- Sustained release Morphine sulphate tablets, also known as MST
- Administered every 12 hours. Available as 10mg or 30mg tablets (cannot be cut/crushed)
- To start Morphine for opioid naïve patients, give mist Morphine 2.5-5mg q4h and 2.5-5mg p.r.n. (when necessary) up to 1 hourly (i.e. minimum of 1 hour between each dose). If the patient requires more than 3 p.r.n. doses in a 24 hour period, the patient’s pain should be reviewed. Increase the regular q4h mist Morphine dose gradually based on response.
- When pain is controlled, mist Morphine can be converted to MST q12h (e.g. if mist Morphine 10mg q4h was able to control the pain, then it can be converted to MST 30mg q12h).
- If the patient is already on regular weak opioids (e.g. Codeine or Tramadol), use the Opioid Conversion Calculator to determine the appropriate Morphine dose.
Using Fentanyl
- Fentanyl is a safe strong opioid in moderate to severe renal failure
- It is useful in:
- intractable constipation and subacute intestinal obstruction
- dysphagia
- poor compliance
- Doses are the same for transdermal, subcutaneous and intravenous routes.
- Patch strengths come in 12, 25 and 50mcg/hr
- Note lag time of 8-12 hours for analgesia after starting patch and equally the opioids remain in the system for about 8-12 hours after removal of patch
- To start fentanyl in an opioid naïve patient:
- Titrate with short acting opioids (e.g. mist Morphine or Oxycodone normal release) and convert to patch when satisfactory pain control is achieved
- If unsuitable for Morphine or Oxycodone, give a subcutaneous or intravenous infusion of 5-10mcg/hr with a prn breakthrough dose of 1/10 to 1/12 of the total daily dose and titrate according to response before converting to a patch when satisfactory pain control is achieved
- We do not recommend use of Fentanyl patches to titrate pain unless under advice of palliative medicine or pain specialists
- Some organisations use 6mcg/hr (half of the 12mcg/hr patch by peeling off half the sticker) for lower doses, but usage of a “half patch” is not endorsed by the manufacturer.
Using Oxycodone
- May be safer than Morphine in mild to moderate renal failure (but limited data)
- Oral Oxycodone is available in 3 forms:
- Normal release capsules 5mg & 10mg
- Normal release liquid 1mg/ml
- Modified release tablets 10mg & 20mg
- Targin (long acting Oxycodone with oral Naloxone): can be considered for patients with severe constipation despite laxatives.
Undesirable effects of strong opioids
| Undesirable effect |
How to manage |
| Constipation (90%) |
Regular laxatives |
| Nausea and vomiting (30%) |
Regular Haloperidol 0.5-1.5mg at bedtime
Tolerance usually develops in about 1 week |
| Sedation (around 20%) |
Reduce dose, usually mild and self-limiting,
Tolerance usually develops in about a week or so |
| Dry mouth (40%) |
Mouth care |
| Confusion (<1%) |
Reduce dose or switch opioids |
| Hallucinations (<1%) |
Reduce dose or switch opioids |
| Urinary retention (rare) |
Switch opioid |
| Respiratory depression (rare) |
Stop opioid and reassess |
Opioids in renal failure
- Caution is required when estimated creatinine clearance falls below 30ml/min, whether or not a patient is on dialysis
- Fentanyl is recommended in moderate to severe renal impairment
- Oxycodone and Tramadol can be used with caution
- Codeine and Morphine should not be used unless mild renal impairment
Opioids in liver failure
- Fentanyl is the opioid of choice in patients with moderate to severe liver failure or cirrhosis
- Other opioids may be used with caution (by decreasing dose and frequency) and careful monitoring for side effects
What is so bad about Pethidine?
- Pethidine has a toxic metabolite, Norpethidine, which accumulates when Pethidine is given regularly. Particularly in renal impairment, Norpethidine causes tremors, multifocal clonus, agitation, and occasionally seizures.
Adjuvant analgesics
Drugs with a primary indication other than pain, but have analgesic properties in some painful conditions.
- Can play a complementary role to opioids and have opioid sparing effect.
| Drug |
Indication |
| Non-steroidal anti-inflammatory drugs (NSAIDs) |
Inflammatory pain, bone pain |
| Corticosteroids |
Bone pain, raised intracranial pressure, recent onset of neuropathic pain |
Antidepressants
(e.g. Amitriptyline, Nortriptyline, Duloxetine) |
Neuropathic pain |
Anticonvulsants
(e.g. Gabapentin or Pregabalin) |
Neuropathic pain |
| Hyoscine butylbromide |
Colicky or spasmodic pain |
Benzodiazepines
(e.g. Clonazepam or Midazolam) |
Muscle cramps or spasm |
| Bisphosphonates |
Bone pain |
| Lignocaine patch |
Neuropathic pain |
| Ketamine |
Neuropathic pain |
Radiotherapy can also be used for control of bone pain, raised intracranial pressure and neuropathic pain
If symptoms are not controlled with measures outlined here, please consult your local palliative care service.