Duke-NUS MD Curriculum Structure
The Duke-NUS MD Curriculum is modelled after that at Duke University School of Medicine and adapted to suit the Singapore context. It comprises four Phases:
- Phase I: Focuses on basic medical sciences applied to the clinical context
- Phase II: Comprises core clinical clerkships that include Medicine, Surgery, Psychiatry, Neurology, Obstetrics & Gynaecology, and Paediatrics
- Phase III: Features an immersive Research and Scholarship period supplemented by elective and advanced clinical experiences
- Phase IV: Involves advanced clinical education, including summative assessments to ensure work-readiness as a post-graduate year 1 (PGY1) medical trainee
Embedded throughout the curriculum are longitudinal threads, such as Ethics and Professionalism, Clinical Reasoning, Procedural Skills, Patient Safety, Public & Population Health, Data Analytics, Innovation & Design Thinking. These complement the core curriculum and reinforce our comprehensive educational approach.
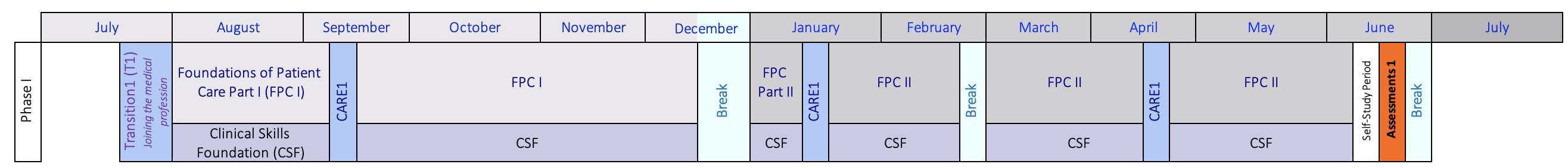
Our refreshed Pre-Clinical curriculum comprises a two-part Basic Science course entitled Foundations of Patient Care (FPC1 & 2), Clinical Skills Foundation, and a longitudinal C.A.R.E. programme that spans the 4-year MD curriculum. This demanding curriculum integrates core biomedical subjects within clinical patient care contexts. In line with Duke University School of Medicine, Duke-NUS streamlines the basic science content into one year, diverging from the traditional two-year span typical of most graduate entry medical schools. Classroom time is viewed as a key opportunity for students to leverage knowledge from preparatory materials, e.g., video-recorded lectures, readings, etc., while fostering capabilities for future leaders, such as teamwork, leadership, and dedication to lifelong learning. To maximize active learning opportunities, we employ a technology-enhanced blended learning model that includes the TeamLEAD instructional method, case-based discussions, and simulation.
| Phase I (Pre-clinical) | - C.A.R.E 1: Joining the Medical Profession
- Foundations of Patient Care (Part 1)
- Foundations of Patient Care (Part 2)
- Clinical Skills Foundation
|
Foundations of Patient Care (FPC)
In FPC1 (Part 1), our students comprehensively explore key disciplines including biochemistry, cell biology, genetics, embryology, anatomy, radiology, microanatomy, physiology, and neuroscience, in an integrated manner.
FPC2 (Part 2) builds upon FPC1, incorporating fundamental concepts of immunology, microbiology, pharmacology, and pathology. This systems-based curriculum is designed to provide a strong grasp of the scientific principles that underpin the structure and function of the human body, and disease mechanisms that lay the foundation for safe medical practice.
The core material is delivered through the TeamLEAD instructional method, a technology-enhanced learning modality, and is supported by laboratory and clinical correlation activities. Notably, through TeamLEAD case studies, students apply newly learned basic science principles to clinical situations. This strategy promotes fundamental clinical reasoning skills and a comprehensive, practical foundation for clinical practice.
Clinical Skills Foundation (CSF)
The CSF course, spanning the entire pre-clinical phase, introduces students to fundamental clinical skills such as history-taking, physical examination, and professional conduct. In history-taking, students develop effective doctor-patient communication skills, emphasizing rapport, active listening, empathy, sensitivity, and respect. Physical examination training covers various organ systems, essential for clinical diagnostic skills. Additionally, the course underlines the importance of ethics and professionalism throughout the learning process.
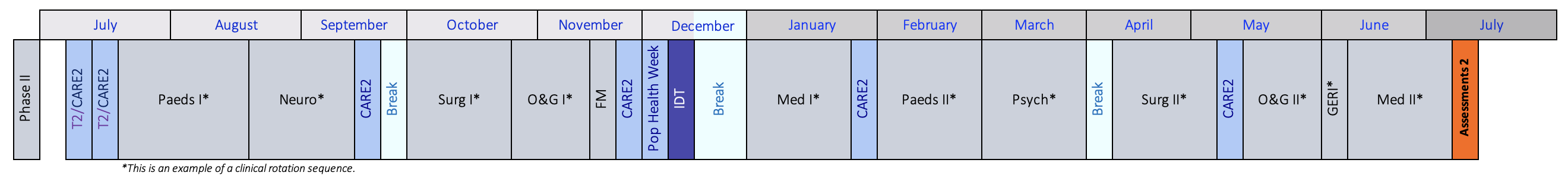
In the second year, students embark on a sequence of core clinical clerkships, gaining extensive exposure to medical specialties including Medicine, Paediatrics, Obstetrics and Gynaecology, Neurology, Psychiatry, Surgery, along with Fundamentals of Family Medicine and Geriatrics. The clerkship phase is structured into two sets of five 4-week rotations (Part I and Part II), providing structured clinical experiences across these diverse fields. Additionally, during this period, students engage in the Research & Critical Thinking and Innovation & Design Thinking components, integral parts of the research and scholarship thread within the curriculum. Alongside these rotations, students participate in the longitudinal C.A.R.E. programme that spans all four years and is designed to enhance clinical skills and complementing capabilities to prepare students for safe practice of medicine.
| Phase II (Clinical Clerkships) | - C.A.R.E. 2: Learning From & For Patients
- Medicine Clerkship
- Surgery Clerkship
- Paediatrics Clerkship
- Obstetrics & Gynaecology Clerkship
- Neurology Clerkship
- Psychiatry Clerkship
- Geriatrics Medicine
- Fundamentals of Family Medicine
- Research & Critical Thinking
- Innovation & Design Thinking
|
Research & Critical Thinking (RCT)
RCT is meticulously designed to cultivate early research abilities and critical thinking skills, setting the stage for the Research and Scholarship year. This component encourages students to master the art of formulating hypotheses that could substantially contribute to both knowledge enhancement and patient care improvement. It also covers designing effective studies and interpreting statistical outcomes. By closely integrating with clinical clerkships throughout the year, RCT effectively bridges the gap between theoretical knowledge and its practical application, emphasizing evidence-based practice and clinical relevance.
Innovation & Design Thinking (IDT)
IDT aims to inspire students to adopt a creative and scholarly approach to addressing healthcare challenges. Through engaging activities such as a hackathon dedicated to tackling healthcare challenges, students are introduced to a wide array of scientific methodologies and design thinking processes. They are guided to devise and prototype innovative solutions, ranging from products and devices to technologies and processes, aimed at resolving specific healthcare issues. Additionally, IDT encompasses discussions on key entrepreneurial and regulatory aspects vital for safeguarding intellectual property and transitioning prototypes into market-ready ventures.
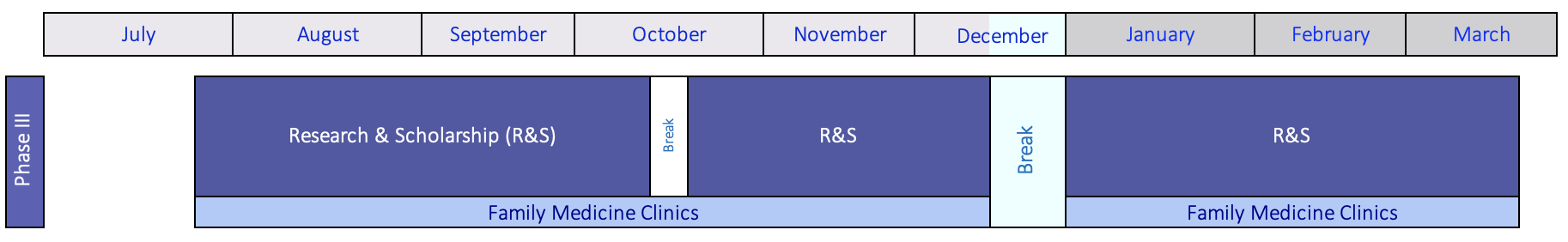
The Duke-NUS curriculum showcases a distinctive, vertically-integrated research thread. It starts with foundational concepts in Phase I and continues with further development throughout Phase II. This preparation paves the way for a 9-month immersive mentored-research experience in Phase III, culminating in a thesis submission. Students select a research area that aligns with their interests and pursue a project under the mentorship of a self-selected academic mentor. This research can be conducted either locally or at Duke University in North Carolina, USA, offering a diverse range of research environments. Alongside their research, students also participate in Family Medicine clinics, enriching their experience with practical clinical exposure. The curriculum then progresses to advanced clinical rotations by the end of the Research period, seamlessly integrating research and clinical training.
| Phase III (Research and Scholarship) | - Research/Scholarship
- Family Medicine
|
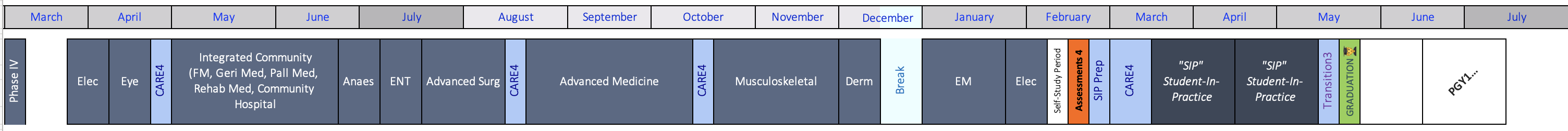
The final phase consists of advanced clinical rotations and provides students with opportunities for increased involvement in patient care, preparing them for heightened responsibilities. This year spotlights various specialties, including Family Medicine, Emergency Medicine (EM), Advanced Surgery, Advanced Medicine, Musculoskeletal rotation (encompassing Orthopaedics, Plastic Surgery, Rheumatology & Immunology), Ophthalmology, Otorhinolaryngology (ENT), Dermatology, Anaesthesiology, and Integrated Community Care. Additionally, students participate in the Student-In-Practice program for Medicine and Surgery, ensuring preparedness for their Post-Graduate Year 1. Elective periods further enable students to explore areas of interest that align with their career aspirations.
| Phase IV (Advanced Clinical Rotations) | - Family Medicine Clerkship
- C.A.R.E. 4: Caring For Patients
- Advanced Medicine
- Advanced Surgery
- Musculoskeletal Rotation
- Emergency Medicine
- Ophthalmology
- Otorhinolaryngology (ENT)
- Dermatology
- Anaesthesiology
- Integrated Community Care
- Student-In-Practice (Medicine)
- Student-In-Practice (Surgery)
- Electives
|
Reflecting the concepts of “Clinician Plus", C.A.R.E. – Connect, Assimilate, Reflect, Explore – is a multi-faceted longitudinal programme that spans the 4-year Duke-NUS MD Curriculum serving as its backbone and aims to complement student learning as they progress in medical school to prepare for safe and capable practice of medicine in an evolving healthcare environment.
The direction of C.A.R.E. across the years is reflected in the theme of the “Transition” periods occurring at the starts of Phase I and II, and end of Phase IV, respectively: Joining the medical profession (T1); learning from and for patients (T2); and caring for patients (T3). The overarching focus of T1 & C.A.R.E.1 as students join the medical community is on Personal and Professional Development, complementing the technical skills they learn in other courses and underscoring adaptive skills critical to thriving in the profession. This is done through opportunities to explore concepts such as emotional intelligence, mindset, teamwork, feedback, critical reflection, conflict management and resilience, along with exploration of Ethics and Professionalism concepts, all the while progressively building on clinical skills.
With entry into clinical medicine, T2 & C.A.R.E.2 become a platform to practice core clinical skills in small groups, guided by a dedicated cohort of faculty. This takes place through threads including Ethics & Professionalism, Core Clinical Reasoning, Procedural skills, Radiology, ECG Interpretation, and Nutrition care. Students explore core tenets of Patient Safety, while participating in Reflective Practice to make sense of the evolving identity. In conjunction with clinical skill development, the programme introduces students to broader themes aligned with healthcare needs, including appreciation for Global, Public and Population Health.
In the final year, students will assume increasingly more patient care responsibilities. Accordingly, C.A.R.E.4 & T3 features more advanced learning opportunities using role-play and simulation to help consolidate knowledge and enhance clinical skills in domains of communication, procedural skills, ethics & professionalism, reflective practice, and systems-based practice, in the runway toward graduation.
Throughout the Duke-NUS MD programme, the core threads provide a scaffold that supports our students' development. These threads are woven into each aspect of the program, ensuring that students acquire a well-integrated set of patient care capabilities enhanced by C.A.R.E. organizing principles to Connect, Assimilate, Reflect, and Explore.
| C.A.R.E. Programme |
| CONNECT with a safe community of learning and professional practice, supported by longitudinal relationships with senior clinical faculty & peers |
| ASSIMILATE medical knowledge and progressively integrate this into clinical practice |
| REFLECT critically on experiences as part of clinical practice and professional identify formation. |
| EXPLORE key healthcare priority areas including how professionals approach, manage and address real world challenges through principles and practices of patient safely, human factors, quality improvement, health transformation, public health, & health promotion |