Back
Friday, 21 Aug, 2020
Researchers in Singapore discover new SARS-CoV-2 variant that causes less severe infections
- The new variant has a large deletion in its genome that removed the ORF8 gene
- Patients infected with the deletion variant virus were significantly less likely to develop severe COVID-19 when compared with the wildtype1 virus
- Findings from the study suggest new avenues for vaccine development and that treatments targeting the ORF8 protein may be effective
The National Centre for Infectious Diseases (NCID), A*STAR’s Singapore Immunology Network (SIgN) and Duke-NUS Medical School today announced research findings that COVID-19 patients infected with a new variant of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) had better clinical outcomes, including a lower proportion of patients developing low blood oxygen (hypoxia) or who required ICU care.
A SARS-CoV-2 variant with a large deletion in its genome was detected in a cluster of infections that occurred from January to March 2020. This variant was first detected in travellers who arrived in Singapore and Taiwan from Wuhan, China suggesting it arose there. In Singapore the virus was transmitted from person-to-person across several clusters before being contained.
The deletion removed 382 nucleotides (Δ382) in a part of the genome which codes for the open reading frame 8 (ORF8) protein. Similar deletions were also detected with SARS in 2003, but the exact function of this protein is obscure. Laboratory studies with the Δ382-variant of SARS-CoV-2 indicate that despite the deletion this virus was not defective and replicated similarly to the wildtype virus.2
131 Individuals who had been infected with either the Δ382-variant or wildtype virus and joined NCID’s PROTECT study were studied.3 PROTECT is a prospective observational cohort study done at seven public hospitals in Singapore – NCID, Singapore General Hospital, National University Hospital, Ng Teng Fong General Hospital, Changi General Hospital, Alexandra Hospital, and Khoo Teck Puat Hospital. Among them, 92 were infected with the wild-type virus only and 39 with the Δ382-variant.
Recognising the significance of the study, the findings were recently published in international scientific journal The Lancet. Riding on the PROTECT cohort, NCID formulated the clinical studies, collected the biological samples and clinical data, while A*STAR's SIgN performed the immunoassays and analysed the immune responses and Duke-NUS Medical School characterised the virus. The study was funded by the National Medical Research Council COVID-19 Research Fund, which is supported by the National Research Foundation Singapore (NRF) and the Ministry of Health (MOH).
“This is indeed a multi-disciplinary collaborative effort applying basic research findings to the clinical setting to demonstrate the difference in clinical phenotypes and the ability to correlate host immunological response to the different strains of SARS-CoV-2 virus. It is expected that the virus will mutate over time and that this may lead to changes in its characteristics. This study demonstrated that the Δ382-variant of SARS-CoV-2 led to a milder form of clinical illness and elicited a more robust immune response. It also underscores the importance to have in place a system to monitor genetic evolutionary changes over time and to study the impact of such changes on human hosts.”, said Professor Leo Yee Sin, Executive Director of NCID.
Key findings of the study reveal that:
- Clinical outcomes were considerably better in patients infected with the Δ382-variant than with the wildtype virus. No patients required supplemental oxygen or ICU care in the Δ382-variant only group.
- Individuals infected with this variant had less systemic release of proinflammatory cytokines and lower levels of growth factors associated with lung injury.
- Analysis also revealed that patients infected with the Δ382-variant had more effective T-cell responses and platelet regulation during the early phase of the infection. T-cell responses correlate with disease severity in COVID-19.
ORF8 is a hotspot for coronavirus mutation, and while this Δ382 variant appears to have been contained, viruses with other ORF8 deletions have been reported from Europe, Australia and Bangladesh. The observed attenuated clinical features suggest ORF8 is a possible target for therapeutic intervention, as well as suggesting possibilities for vaccine development:
- As deletions in the ORF8 region are associated with less severe infections, inhibition of ORF8 function is a possible target for therapeutic intervention and could be a strategy to improve immune surveillance of SARS-CoV-2.
- The deletion virus could be a route to developing a controlled human infection model which will be useful for studying the efficacy of a vaccine.
- The repeated emergence of SARS-CoV-2 viruses with a deletion in ORF8 suggests this region is important for viral adaptation to humans. If antibodies to ORF8 are part of the reason why these viruses keep emerging, this may be a useful target for vaccines to trigger immunity to.
“One of the COVID-19 puzzles we have been trying to solve is why some of our patients get sick while some have only a mild illness. Most of our clinical research efforts have focused on the role of patient factors such as age and chronic medical conditions. Whether different virus types are also important has been much debated, but till now good evidence was lacking. Discovery of this deletion variant and that it had such as profound effect on the infection course is very exciting,” said Dr Barnaby Young, Consultant at NCID and Clinical Lead for the PROTECT study.
"Deletions in ORF8 were commonly detected during the previous SARS outbreak, which provided a basis for studying this virus variant of SARS-CoV-2. The research community is investigating these variants to improve our understanding of SARS-CoV-2 and disease pathogenesis for the development of treatments and vaccines," said Professor Lisa Ng, Senior Principal Investigator, Singapore Immunology Network (SIgN), A*STAR.
Referencing an earlier published study that revealed this evolution of the SARS-COV-2 virus, Prof Gavin Smith, from the Emerging Infectious Diseases Programme at Duke-NUS Medical School, said, "These studies provide the first convincing data showing that an observed genetic change (mutation) in SARS-CoV-2 has affected the severity of disease in patients. In our initial genetic study, we reported a large deletion in the ORF8 gene of SARS-CoV-2 and thought that this could lead to less severe disease in humans through an altered immune response. Comparing data from patients infected with the viruses that have this ORF8 gene deletion confirmed this hypothesis and provided additional insight into its effects on disease progression and immune response. This further highlights the importance of tracking the genetic diversity of SARS-CoV-2 as the virus continues to evolve."
Further studies to understand the function of the ORF8 protein and the effects removing this protein have at the cellular level and the immune response to infection are ongoing.
 | 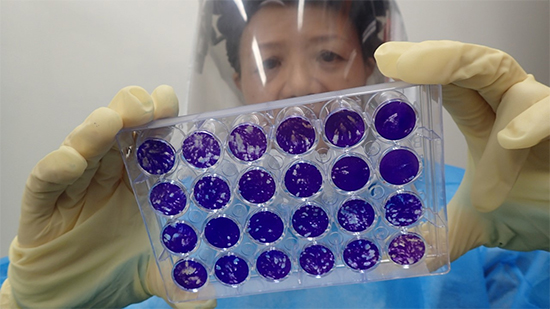 |
A scientist at Duke-NUS Medical School’s Animal Biosafety Level 3 (ABSL3) laboratory prepares to centrifuge samples for viral plaque assays – the standard method for determining virus concentration in terms of infectious dose. | The result of the viral plaque assay is analysed.
|
2 Su, Y., Anderson, D., Young, B., Linster, M., Zhu, F., & Jayakumar, J. et al. (2020). Discovery and Genomic Characterization of a 382-Nucleotide Deletion in ORF7b and ORF8 during the Early Evolution of SARS-CoV-2. Mbio, 11(4). doi: 10.1128/mbio.01610-20